MEDICARE ACCESS & CHIP REAUTHORIZATION ACT
UNDERSTANDING MACRA, MIPS, AND
ALTERNATIVE PAYMENT METHODS
MACRA repeals the Medicare Part B Sustainable Growth Rate (SGR) reimbursement formula and replaces it with a new value-based reimbursement system called the Quality Payment Program (QPP). The quality payment program has two tracks healthcare organizations can choose from:
MEDICARE ACCESS & CHIP REAUTHORIZATION ACT
UNDERSTANDING MACRA, MIPS, AND
ALTERNATIVE PAYMENT METHODS
MACRA repeals the Medicare Part B Sustainable Growth Rate (SGR) reimbursement formula and replaces it with a new value-based reimbursement system called the Quality Payment Program (QPP). The quality payment program has two tracks healthcare organizations can choose from:
THE MERIT-BASED INCENTIVE PROGRAM (MIPS)
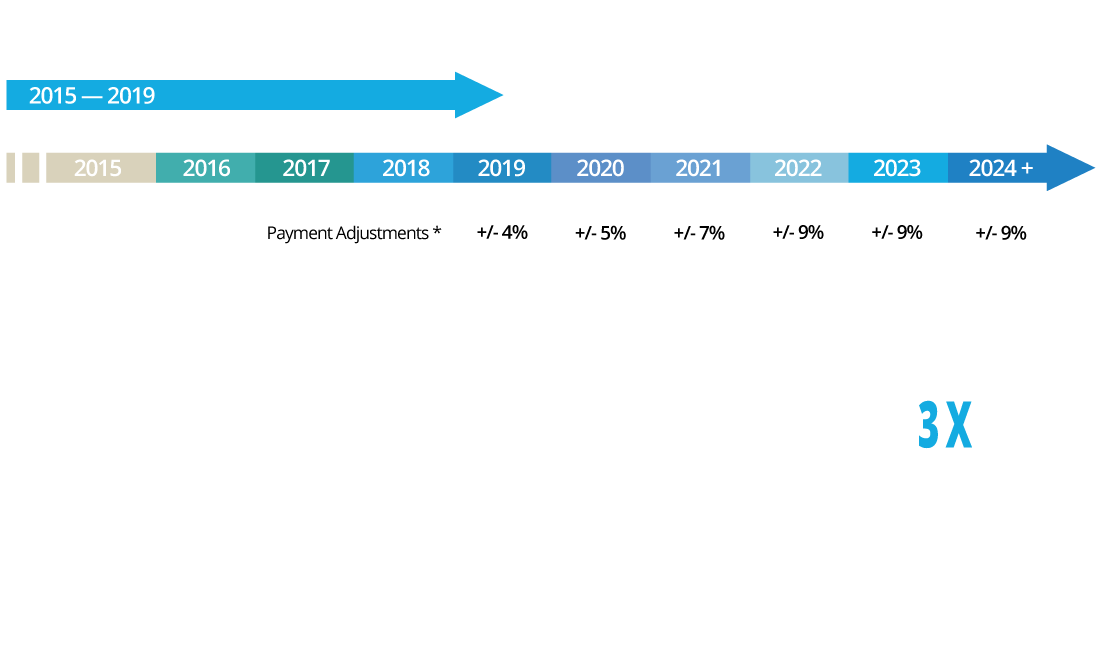
In MIPS, you earn a payment adjustment based on evidence-based and practice-specific quality data. Based on your performance, you will see a positive, neutral, or negative adjustment to your Medicare payments for covered professional services.
ALTERNATIVE PAYMENT MODEL (APMs)
An Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
PERFORMANCE-BASED PAYMENTS
MIPS STREAMLINES THREE
HISTORICAL MEDICARE
PROGRAMS
MIPS combines the existing Physician Quality Reporting System (PQRS), the Value-based Payment Modifier (VM) Program and the Medicare Electronic Health Record (EHR) Incentive Program (Meaningful Use) — into a single payment program.
WHO MUST PARTICIPATE?
Eligible Clinicians who: Bill Medicare $30,000 a year, provide care for 100 Medicare patients a year. Clinicians (Physician, Physician assistant, Nurse practitioner, Clinical nurse specialist, Certified registered nurse anesthetist.
WHEN DOES MIPS START?
Providers have between January 1, 2017 and October 2, 2017 to begin reporting their data.
PERFORMANCE-BASED PAYMENTS
MIPS STREAMLINES THREE
HISTORICAL MEDICARE
PROGRAMS
MIPS combines the existing Physician Quality Reporting System (PQRS), the Value-based Payment Modifier (VM) Program and the Medicare Electronic Health Record (EHR) Incentive Program (Meaningful Use) — into a single payment program.
WHO MUST PARTICIPATE?
Eligible Clinicians who: Bill Medicare $30,000 a year, provide care for 100 Medicare patients a year. Clinicians (Physician, Physician assistant, Nurse practitioner, Clinical nurse specialist, Certified registered nurse anesthetist.
WHEN DOES MIPS START?
Providers have between January 1, 2017 and October 2, 2017 to begin reporting their data.
Only time will tell how the public release of the MIPS score will impact providers.VIGILANCE HEALTH
The question is “how will it affect your organization’s reputation
and ultimately – the bottom line.”
Only time will tell how the public release of the MIPS score will impact providers. The question is “how will it affect your organization’s reputation and ultimately – the bottom line.”VIGILANCE HEALTH
MEASURING PERFORMANCE
CALCULATING A COMPOSITE
PERFORMACE SCORE
CMS is instituting a “unified scoring system” for MIPS that differs from how previous Medicare quality programs were evaluated in several ways:
1.) Measures and performance in each MIPS performance category will be converted to points
2.) Eligible clinicians will know in advance what they need to submit to achieve top performance
3.) Partial credit is available.
The MIPS unified scoring system results in calculating a Composite Performance Score for all participating clinicians that represents performance in the four categories on a scale of 0-100 points. Each performance category is assigned a weighted value, which can change each performance year.
The MIPS scoring methodology is also intended to take into account situations of exceptional performance, evaluation at the group or individual provider performance level, and the special circumstances of small practices, practices located in rural areas, and non-patient-facing MIPS eligible clinicians.
MEASURING PERFORMANCE
CALCULATING A COMPOSITE
PERFORMACE SCORE
CMS is instituting a “unified scoring system” for MIPS that differs from how previous Medicare quality programs were evaluated in several ways:
1.) Measures and performance in each MIPS performance category will be converted to points
2.) Eligible clinicians will know in advance what they need to submit to achieve top performance
3.) Partial credit is available.
The MIPS unified scoring system results in calculating a Composite Performance Score for all participating clinicians that represents performance in the four categories on a scale of 0-100 points. Each performance category is assigned a weighted value, which can change each performance year.
The MIPS scoring methodology is also intended to take into account situations of exceptional performance, evaluation at the group or individual provider performance level, and the special circumstances of small practices, practices located in rural areas, and non-patient-facing MIPS eligible clinicians.
WINNING STRATEGY
WHAT ARE THE
FINANCIAL IMPACTS?
The potential MIPS incentives and penalties via value-based payment adjustments are substantial. The financial
impacts of these scores can amount to millions of dollars per organization and will significantly grow over the
course of the next several years. Penalties assessed for poor performance or noncompliance will be used to
fund incentive payments for high performers, so the “winners” effectively will be paid by the “losers.”
WINNING STRATEGY
WHAT ARE THE
FINANCIAL IMPACTS?
The potential MIPS incentives and penalties via value-based payment adjustments are substantial. The financial impacts of these scores can amount to millions of dollars per organization and will significantly grow over the course of the next several years. Penalties assessed for poor performance or noncompliance will be used to fund incentive payments for high performers, so the “winners” effectively will be paid by the “losers.”
PUBLISHED RESULTS
WHAT ARE THE
REPUTATIONAL IMPACTS?
MIPS will publish on a website each eligible clinician’s annual final score and the scores for each MIPS performance category within approximately 12 months after the end of the relevant performance year. For the first time, consumers will be able to see their clinicians rated on a scale of 0 to 100 and how they compare to peers nationally.
The provider’s MIPS score could effect the decision making of individual patients, provider networks, medical staff credentialing, professional liability insurance, among other things.
PUBLISHED RESULTS
WHAT ARE THE
REPUTATIONAL IMPACTS?
MIPS will publish on a website each eligible clinician’s annual final score and the scores for each MIPS performance category within approximately 12 months after the end of the relevant performance year. For the first time, consumers will be able to see their clinicians rated on a scale of 0 to 100 and how they compare to peers nationally.
The provider’s MIPS score could effect the decision making of individual patients, provider networks, medical staff credentialing, professional liability insurance, among other things.
POSITIVE ADJUSTMENTS
TOP PERFORMERS
WILL BE REWARDED
In 2017, a Composite Performance Score of three points will ensure that an eligible clinician or group will avoid a negative payment adjustment. Three points can be earned by reporting at least one quality measure, at least one improvement activity, or all five base measures in the Advancing Care Information category.
Though it is relatively easy to avoid a negative payment adjustment in the 2017 (more difficult in 2018 and beyond), there is still a reason to strive for stellar performance. Exceptional performers who achieve a MIPS Composite Performance Score of at least 70 out of 100 will be eligible for an additional positive adjustment from a bonus pool of $500 million.
POSITIVE ADJUSTMENTS
TOP PERFORMERS
WILL BE REWARDED
In 2017, a Composite Performance Score of three points will ensure that an eligible clinician or group will avoid a negative payment adjustment. Three points can be earned by reporting at least one quality measure, at least one improvement activity, or all five base measures in the Advancing Care Information category.
Though it is relatively easy to avoid a negative payment adjustment in the 2017 (more difficult in 2018 and beyond), there is still a reason to strive for stellar performance. Exceptional performers who achieve a MIPS Composite Performance Score of at least 70 out of 100 will be eligible for an additional positive adjustment from a bonus pool of $500 million.